Episodes

Sunday May 08, 2022
Virtual Interviewing and Transitioning into Residency
Sunday May 08, 2022
Sunday May 08, 2022
Interviewing and beginning your career in medicine comes with challenges! Dr. Sarah Bunting, MD is a PGY-1 emergency medicine resident at Maine Medical Center. Listen in to hear her advice on transitioning from medical school to residency, virtual interviewing, and what to look for in a residency!
For the full show notes, click here.
Hallie Bates, MSIV and Alex Schin, MSIV
Peer Reviewed by Lauren Wendell, MD and Jeffrey A. Holmes, MD

Thursday Jun 24, 2021
OMG, TMI! What does open notes mean for you and your patients?
Thursday Jun 24, 2021
Thursday Jun 24, 2021
The 21st Century CURES act has mandated that starting on April 5th, 2021 patient notes (with a few very narrow exceptions) must be easily available to patients via their patient portal. How did this come about, and what does it mean for us?
Click Here for full show notes
This lecture was presented at the 2021 Maine Medical Center Winter Symposium. For more information on the symposium click here.
Sam Wood, MD
Monday Jun 07, 2021
NOT A STAB IN THE DARK - MASTERING ULTRASOUND GUIDED PERIPHERAL IV
Monday Jun 07, 2021
Monday Jun 07, 2021
Ultrasound Jedi, Dr. Andrew Fried, takes us through a masterclass on placing ultrasound guided peripheral IV's.
For full show notes, check out our blog post on Down East EM.
Jeffrey A Holmes, MD
Monday Apr 05, 2021
Two STEMI Mimics You've Got to Know!
Monday Apr 05, 2021
Monday Apr 05, 2021
This year we are very fortunate to have Dr. Amal Mattu, EKG Jedi, as teaching faculty for our 39th Maine Medical Center/Maine ACEP Winter Symposium. In this lecture, he helps us differentiate septal STEMIs from other potentially life threatening mimics.
To check out our virtual 39th Winter Symposium, check out the conference website at www.mmcwintersymposium.com
Jeff Holmes, MD

Wednesday Mar 24, 2021
Pediatric Diarrhea with Dr. Jay Larmon
Wednesday Mar 24, 2021
Wednesday Mar 24, 2021
Kids poop. Most of the time it goes well- aside from the messes and the wipes and the cleaning and the change of clothes. But sometimes medically pediatric diarrhea is not alright. In this interview with pediatrician Dr. Jay Larmon we go over the spectrum of pediatric diarrhea, from the a-okay to the not-so-right and everything in between.
Check out our blog post for more.
Authors: Jason Hine MD and Jay Larmon MD
Peer Review: Jeff Holmes MD and Mike Burla MD
Wednesday Mar 03, 2021
Academics for the Community Provider- Bringing quality and longevity to your career
Wednesday Mar 03, 2021
Wednesday Mar 03, 2021
In medicine we often draw a solid line between community and academic medicine, but this likely is a fallacy. In fact there is a huge amount of academia that can be found and thrive in a community hospital. In this interview we talk with Dr. Salim Rezaie of the REBEL EM blog and podcast, a man who has walked both sides of this imaginary line between community and academics. In our chat we discuss ways to get involved in academics in the community and the vast array of rewards that come with that including improved patient care, increased fervor for your work, decreased burnout, and increased career longevity.
Authors: Jason Hine MD, Salim Rezaie MD
Peer Review: Jeff Holmes MD, Mike Burla MD
Thursday Jan 07, 2021
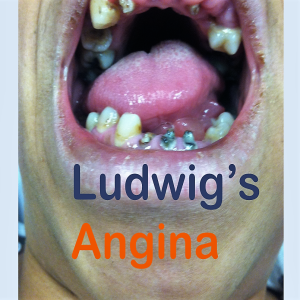
Ludwig's Angina- more than a toothache
Thursday Jan 07, 2021
Thursday Jan 07, 2021
In this episode we dive into the nasty, gnarly infection that is Ludwig's Angina. It's a bad player- and with complications including mediastinitis, epiglottitis, and asphyxiation- it's one you need to know. In this vodcast we highlight a case of Ludwig's Angina, showing some important images and videos of the presentation, and dive into the finer points of the disease.
Check out our blog for shownotes, references, and more
Author: Jason Hine MD
Peer Review: Dr. Jeff Holmes and Dr. Mike Burla
Saturday Dec 12, 2020
Saturday Dec 12, 2020
This is Part 2 of our discussion of the COVID-19 vaccines. With frontline providers across the country (and world) asking themselves "Am I comfortable getting this vaccine?" we thought it important to review some of the basic science (Part 1) and data (Part 2) behind these mRNA vaccines.
In this podcast we ask
What did the Pfizer phase 3 study show?
What outcomes did they look at?
Did they meet those outcome targets?
Specifically- what the vaccine effective ... and was it safe?
Disclaimer: I am not an infectious disease physician, immunologist, or population health specialist. These perspectives are those of an Emergency Medicine physician. In order to expedite the delivery of this material to you, the frontline provider, this content did not undergo our typical peer review process.
References:
Rabies vaccine phase 1 study [pubmed]
Pfizer Phase 3 study results [NEJM]
Check out the DownEast EM site for more.
Author: Jason Hine MD
Friday Dec 11, 2020
The COVID 19 Vaccine- What the front line provider needs to know
Friday Dec 11, 2020
Friday Dec 11, 2020
This is Part 1 of our discussion of the COVID-19 vaccines. With frontline providers across the country (and world) asking themselves "Am I comfortable getting this vaccine?" we thought it important to review some of the basic science (Part 1) and data (Part 2) behind these mRNA vaccines.
In this podcast we ask
What exactly is an RNA vaccine?
How do they work?
Is the COVID-19 vaccine the first of these types of vaccines?
among many others
Disclaimer: I am not an infectious disease physician, immunologist, or population health specialist. These perspectives are those of an Emergency Medicine physician. In order to expedite the delivery of this material to you, the frontline provider, this content did not undergo our typical peer review process.
References:
Rabies vaccine phase 1 study [pubmed]
Pfizer Phase 3 study results [NEJM]
Check out the DownEast EM site for show notes.
Author: Jason Hine MD
Friday Dec 04, 2020
Friday Dec 04, 2020
They have something DOWN THERE... No surprises, it's herpes. But making the diagnosis is the just first of many issues and questions- how do you treat it? Will it come back? How do I stop from spreading it to other partners? Is there something I can do to decrease my number of outbreaks? All great questions we should be ready to answer. In this vodcast Dr. Leger reviews this disease and these important questions.
Check out our Down East EM blog for references and a whole lot more amazing content.
Author: Dr. Janessa Leger MD
Peer Review: Dr. Jason Hine MD and Dr. Jeff Holmes MD